THE VARIATIONS IN ELECTRICAL CARDIAC SYSTOLE AND ITS IMPACT ON SUDDEN CARDIAC DEATH.
Before anything else, is essential to define what is the electrical cardiac systole. Especially when there are so many discrepancies among different authors.
Includes cardiac electrical systole from the beginning of the P wave (atrial depolarization) to the end of the T wave (ventricular repolarization).
Would cover thus the P wave, PR interval, QRS complex, ST segment, T wave.
For other authors, this one only would include from the beginning of QRS complex to the end of the T wave.
There are several changes, especially in its length, that can cause a sudden death in case that they are not adequately diagnosed and, thus, with the properly treated.
STANDARD VALUES (in length)
P-wave: 0.06-0.09 seconds in length.
PR- interval: 0.12 to 0.20 seconds in length.
QRS- complex: 0.06 to 0.10 seconds in length.
QT- interval (corrected): 0.40 to 0.44 seconds in length.
RR- interval: 0.60-1.00 seconds in length.
Normal duration of cardiac electric systole: 35-45% of total duration of the cardiac cycle (R-R interval)
(The length of cardiac electrical systole is considered normal until reaching 45% of the overall length of cardiac cycle: a greater value is considered as prolonged and lesser is considered as shortened)
The sudden death is defined for most authors as a natural death that happens very instantaneously or within the first hour from the beginning of the symptoms, in a patient with well-known previous disease or without her, but is unexpected totally. Although we do not agree with some nuances of such definition, we will give it as acceptable. Consequently, any sudden death should be considered either of cardiac origin when the heart is the affected organ, structurally or without macroscopic alterations of its structure.
The cardiac problems are the main cause of unexpected death. It is estimated that occurs about 1 case of sudden death for every 100,000 young athletes each year (under 35). Even though exercise is beneficial for health, sport of competition increases the risk of sudden death.
TABLE 1.- The most frequent causes of sudden death in overall.
Cardiac commotion.
Coronary artery anomaly.
Left ventricular hypertrophy of undetermined cause.
Myocarditis.
Rupture of aortic aneurysm.
Arrhythmogenic right ventricular cardiomyopathy.
Bypass coronary artery.
Aortic valve stenosis.
Atherosclerotic disease of the coronary artery.
Dilated cardiomyopathy.
Myxomatous mitral degeneration.
Asthma.
Heatstroke.
Drug Abuse.
Other cardiovascular causes.
Long QT Syndrome.
Ruptured brain aneurysm.
Cardiac sarcoidosis.
Traumatic cardiac injury.
The three most common causes for sudden cardiac death are:
Hypertrophic cardiomyopathy. (HCM) (Figure 1):
It is a disease of the myocardium in which a portion of the myocardium is hypertrophied (thickened) without any obvious cause. It is perhaps most well-known as a leading cause of sudden cardiac death in young athletes. The occurrence of Hypertrophic cardiomyopathy is a significant cause of sudden unexpected cardiac death in any age group and as a cause of disabling cardiac symptoms. Younger people are likely to have a more severe form of Hypertrophic cardiomyopathy. HCM is frequently asymptomatic until sudden cardiac death, and for this reason, some suggest routinely screening certain populations for this disease.
A cardiomyopathy is a primary disease that affects the muscle of the heart. With Hypertrophic cardiomyopathy (HCM), the sarcomeres (contractile elements) in the heart replicate causing heart muscle cells to increase in size, which results in the thickening of the heart muscle. In addition, the normal alignment of muscle cells is disrupted, a phenomenon known as myocardial disarray. HCM also causes disruptions of the electrical functions of the heart. HCM is most commonly due to a mutation in one of 9 sarcomeric genes that results in a mutated protein in the sarcomere, the primary component of the myocyte (the muscle cell of the heart).
While most literature so far focuses on European, American, and Japanese populations, HCM appears in all racial groups. The prevalence of HCM is about 0.2% to 0.5% of the general population.
Arrhythmogenic right ventricle cardiomyopathy. (Figure 2)
Arrhythmogenic right ventricular dysplasia (ARVD), also called arrhythmogenic right ventricular cardiomyopathy (ARVC) or arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C), is an inherited .Heart disease ARVD is caused by genetic defects of the parts of heart muscle known as desmosomes, areas on the surface of heart muscle cells which link the cells together. The desmosomes are composed of several proteins, and many of those proteins can have harmful mutations. The disease is a type of non-ischemic cardiomyopathy that involves primarily the right ventricle. It is characterized by hypokinetic areas involving the free wall of the right ventricle, with fibro fatty replacement of the right ventricular myocardium, with associated arrhythmias originating in the right ventricle. ARVD is often found in association with diffuse palmo-plantar keratoderma, and woolly hair, because their genes are nearby and often inherited together.. ARVC/D is an important cause of ventricular arrhythmias in children and young adults. It is seen predominantly in males, and 30-50% of cases have a familial distribution.
Arrhythmogenic sudden death syndrome:
It is a generic name that includes many alterations in cardiac electrical conduction
capable of produce instant death. This syndrome includes all sudden cardiac
deaths wherein the cause of death could not be diagnosed, even after the
necropsy. It is the cause of more 5% of all sudden cardiac deaths.
That is, if we discard the non-cardiac causes and structural heart problems, this
problem is denominated as arrhythmogenic sudden death syndrome from a
generic form.
As the diagnostic techniques are being more appropriate each day, these numbers
grows exponentially.
Here, would be included all events from our chapter proposal : Alterations in electrical cardiac systole and its impact on sudden cardiac death.
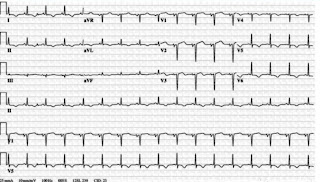
Figure 1.
ECG is abnormal., 80-90% of cases. Abnormal Q-waves in inferior leads. Increasing the voltage in medium or left precordial (V3-V6). ST segment depression, negative T- waves in precordial leads, middle and left. Less often: Increasing in the left atrium, left axis, Giant negative T waves, atrial fibrillation, ventricular extra-systoles, ventricular tachycardia in severe cases.
Figure 2
90% of individuals with ARVD have some EKG abnormality. The most common EKG abnormality seen in ARVD is T wave inversion in leads V1 to V3. However, this is a non-specific finding, and may be considered a normal variant in right bundle branch block (RBBB), women, and children under 12 years old. RBBB itself is seen frequently in individuals with ARVD. This may be due to delayed activation of the right ventricle, rather than any intrinsic abnormality in the right bundle branch. The epsilon wave is found in about 50% of those with ARVD. This is described as a terminal notch in the QRS complex. It is due to slowed intraventricular conduction. The epsilon wave may be seen on a surface EKG; however, it is more commonly seen on signal averaged EKGs. Ventricular ectopy seen on a surface EKG in the setting of ARVD is typically of left bundle branch block (LBBB) morphology, with a QRS axis of -90 to +110 degrees. The origin of the ectopic beats is usually from one of the three regions of fatty degeneration (the "triangle of dysplasia"): the RV outflow tract, the RV inflow tract, and the RV apex.
OTHER DISORDERS IN ELECTRICAL CARDIAC SYSTOLE AS CAUSE FOR SUDDEN CARDIAC DEATH.
As we have said previously, the electrical cardiac systole originates from the beginning of the P wave (atrial depolarization) to the end of the descending branch of the T wave (ventricular repolarization). Are included, therefore, the succession of P-QRS-T and its corresponding intervals and segments: PQ, ST and QT. The mathematical possibilities in the variation on length of electrical systole of the heart may be several. It is well documented and demonstrated that such changes in length can cause that be more vulnerable and unstable all myocardial cells, and can also cause serious cardiac arrhythmias, several syncope episodes and even sudden death for this motive. Even today, many of these disorders are poorly understood and, too many times, its clinical manifestations are categorized as "episodes of epilepsy"; other times (most) are classified within a "common sack" called "channelopathies”, when -actually- is the alteration from electrical cardiac systole the true etiology of them.
All these disorders can cause syncopal episodes and a sudden cardiac death.
The measures and lengths of the different components of electrical cardiac systole, considered for most authors as normal are these:
PR-interval: 0.120- 0.200 seconds.
QRS complex: 0.08-0.120 seconds.
QT-interval (corrected): 0.350-0.450 seconds. (Here, there is much disagreement among different authors). The most used methods for QT interval correction, since it is frequency-dependent, are Bazett, Fridericia.
When the PR-interval is lesser than 0.120 seconds, we call it a short PR-interval. In contrast, when is greater than 0,200 seconds, we call it a first-degree AV block. When the QRS complex is lesser than 0.08 seconds, we call it "narrow QRS" but when is greater than 0,120 seconds, we call it "wide QRS". Likewise, when the corrected QT- interval length is lesser than 0,350 seconds, we call it Short QT- interval and when is greater than 0,450 seconds, we call it a Long QTc- interval.
It is clear that there may be, in the same ECG recording, a combination of them all.
Some of these disorders, we will explain briefly below.
WOLFF-PARKINSON-WHITE’S SYNDROME (WPWS).
Wolff-Parkinson-White syndrome (WPWS) is a congenital heart disease (PRKAG2. Genetic map 7q36) characterized by a premature ventricular depolarization caused by an abnormal atrioventricular accessory pathway, between the atria and ventricles, known as Kent’s bundle. However, even today, is called into question the real cause of Wolff-Parkinson-White, there are some authors who believe that, PRKAG2 mutations, are caused by a glycogen storage cardiomyopathy associated with WPWS, because the overwhelming majority of accessory pathways occur in individuals without structural heart disease, and probably without this mutation. The pathogenesis of accessory pathway formation in PRKAG2 may be completely different, and some authors believe it is due to an inflammation of myocardial cells that occur in the atrial-ventricular connections.
In fact, do not even know if the accessory pathways are mediated genetically or due to environmental exposures or randomly.
A short PR interval, a delta wave, a wide QRS complex (greater than 120 ms) and, occasionally, alterations in the ventricular repolarization are its main electrocardiographic characteristics on the ECG. Its incidence varies between 0, 1% and 3% in the general population.
It is essential to achieve the right differential diagnosis between:
Wolff-Parkinson-White’s syndrome or real ventricular pre-excitation.
Lown-Ganong-Levine syndrome or accelerated atrioventricular conduction.
Mahaim’s syndrome.
“Short PR alongside short QT” intervals in the same person. (Breijo's Pattern).
Typical ECG image of the Wolff-Parkinson-White.
.
In this context of ECG recording, that has a normal heart rate, a short PR interval, a delta-wave and an early ventricular repolarization can be seen.
LOWN-GANONG-LEVINE SYNDROME (LGL).
This syndrome was described in 1952 by Lown, Ganong, and Levine, forming the famous now used to describe it. It is considered a preexcitation syndrome.
We now know four types of pre-excitation syndrome:
Wolff-Parkinson-White or ventricular preexcitation true.
Lown-Ganong-Levine or accelerated atrioventricular conduction.
Short PR alongside short QT” intervals in the same person. (Breijo's Pattern).
Mahaim Syndrome.
LGL is a disease entity that is included within the more general condition called Short PR-Interval).
Etiology
• Acquired .
• Congenital :
I. Inherited.
II. Not inherited.
The familial form is inherited, as an autosomal dominant genetic trait has been associated with the PRKAG2 gene that encodes the activated AMP protein kinase, responsible for transport and store energy from the heart. A mutation in this gene could explain the susceptibility of the heart to the crises of tachycardia. Mutation has been identified on the long arm of chromosome 7 (7q34-q36).
The Lown-Ganong-Levine may affect approximately 1 in every 50,000 people.
Several structural abnormalities have been proposed as the possible basis for LGL, including the presence of James's fibbers, Mahaim's fibbers, Brechenmacher and underdeveloped anatomic sinus node (hypoplastic).
Each of these fibbers can only be identified histologically.
Thus, unless other studies demonstrate definitive- structural or functional -abnormalities, the diagnosis of LGL remains a clinical diagnosis.
In the absence of significant structural heart disease, the mortality rate appears to be very low.
Patients may present with an acute episode of tachycardia or a history of symptoms suggestive of paroxysmal tachycardia.
In diagnosis is necessary to make:
1. A standard test for tachycardia, including an ECG to document the rhythm.
2. Serum electrolytes, calcium, magnesium levels, and levels of serum thyroid hormone-stimulating hormone (TSH). Lithemy.
3. History suggestive of recurrent paroxysms of tachycardia,
4. A Holter monitor or event recorder may be useful to document the rhythm during acute symptomatic episodes.
5. An ergometric study.
6. In rare cases, an implantable monitor for pace may be helpful.
7. Family History. (Screening).
Differential Diagnosis with Wolf-Parkinson-White
Although apparently similar, there are differences, which, in our opinion, are critical with respect to drug treatment elective. The key differences are:
-The LGL is a PR- interval shortened due to, the presence of accessory pathway, prevents the AV node but normal QRS because the accessory pathway (James fibbers) binds directly to the sinus and depolarizes the ventricles not directly, but does so by typical pathway, by the Hiss-Purkinje system.
- Not displayed "Delta waves -" in D1, aVL, V5 and V6.
- The QRS complexes tend to be narrow because there is usually no interventricular conduction disturbance.
- It is not be as frequent the association of atrial fibrillation during concomitant crisis.
Prognosis:
No studies have shown an increased risk of sudden death or reduced survival for patients meeting the criteria for the diagnosis of LGL.
Current Therapeutic Bases
Rarely, the drug medical therapy can have failures usually, but there are patients in who there is not effective (for patients who continue to have recurrent and intolerable symptoms). In such extreme cases are used:
Radiofrequency ablation (RF)..
The external pacemaker.
The Implantable Cardioverter Defibrillators (ICDs).
This destroys the accessory pathway using a catheter (tube) inserted into the body to reach the heart. The success rate of this procedure ranges between 85 and 95% depending on the location of the extra or additional route.
Digoxin, verapamil and beta-blockers (other drugs commonly used to treat other types of tachycardia) can increase the frequency of episodes of tachycardia in some people with this syndrome. Beta-blockers may increase cardiac depression.
We can use drugs such as adenosine (Inpatient), and amiodarone to control or prevent episodes of tachycardia.
For the control of tachycardia is usually proceed according to the severity of the implementation of vagal maneuvers carotid massage type and Valsalva maneuver (forced expiratory made with the nose and mouth closed).
Typical ECG image of the Lown-Ganong-Levine:
.
SHORT PR-INTERVAL ALONGSIDE SHORT QT- INTERVAL ON THE SAME PERSON. (BREIJO'S PATTERN).
In 2006, Breijo-Marquez, Pardo Ríos et al. evaluated a series of young patients, who had had, since childhood, many episodes of nocturnal palpitations, chest pain, full loss of consciousness (syncope), and which were accompanied by tonic-clonic seizures. All had been diagnosed and treated as epileptic episodes. Treatment outcomes were null. They were always considered as normal, in every cardiac studies performed absolutely.
However, all these patients had an ECG recording common:
A PR-interval lesser than 0,120 seconds with a QTc-interval equal to or lesser than 0.350 seconds.
That is, a pattern of short PR and QTc in the same person.
The correct treatment was begun (beta-blockers and, in some cases, an implantable cardio defibrillator, ICD.). Was removed all treatment from epilepsy.
The outcome to date is satisfactory.
Although we don’t know, with certainty, the etiology of this pattern of ECG to date, we know that there were two important confusions:
First. - The physicians mistook to syncopal episode, with an epileptic episode.
Second. - The syncopal episodes are due to a cardiac disorder (was a cardiogenic syncope due to a cardiac electrical systole's alteration).
This ECG recording may be easily confused with a Lown-Ganong-Levine, since both have a short PR-interval. Nevertheless, in this type of ECG pattern there is also a short QTc-interval.
Unfortunately, both entities are confused with epileptic episodes too often.
Sudden cardiac death is extremely frequent in this type of event.
Typical ECG image of the “Short PR alongside short QT” intervals in the same person. (Breijo's Pattern):
This ECG recording was the first with 12 leads that was obtained from our Hospital from Boston. MA. The patient was a 17 years-old male. We can see a shortening of the PR and QT intervals (Bazett), especially in inferior and left precordial leads. PR-interval length is lesser than 0.120 seconds and QTc length is lesser than 0.350 seconds. Patient had the symptoms exposed previously. He was also diagnosed for epileptic episodes. However, he had syncopal episodes by cardiological disturbances
MAHAIM SYNDROME.
Mahaim syndrome is characterized by:
The PR- interval with a standard length. Presence of pseudo-delta wave in the initial phase of the QRS complex because the sinus stimulus enters to AV node where physiological suffers a delay and then depolarizes the ventricles by an abnormal way: Mahaim fibers. That is:
PR-interval with a normal length.
Wide QRS complexes.
Typical ECG image of the Mahaim’s Syndrome
Differential diagnosis among various entities with alterations in electrical cardiac systole.
ENTITY.
PR-interval
QRS complex
QTc -interval
W.P.W
Short.
Wide (δ-wave)
Normal
L.G.L
Short
Normal
Normal
Mahaim
Normal or Short
Normal or wide
Normal
Breijo’s Pattern
Short
Normal
Short
Differential diagnosis, based on the characteristics from the different intervals and complex.
SOME VARIATIONS IN ELECTRICAL CARDIAC SYSTOLE THAT CAN CAUSE SUDDEN DEATH.
(All these examples were discovered by Breijo et al. They are still very underdiagnosed).
Wolff-Parkinson-White and Prolonged“Q-T”Patterns in the Same Electrocardiographic Record
Wolff-Parkinson-White syndrome (WPWS) is a congenital heart disease (PRKAG2. Genetic map 7q36) characterised by a premature ventricular depolarisation caused by an abnormal atrioventricular accessory pathway known as Kent’s bundle. Prolonged QT syndrome (PQTS) consists of an abnormal prolongation of the QT interval on the ECG, which can be both inherited and acquired. This anomaly is known to favour the occurrence of malign cardiac arrhythmias, above all polymorphic ventricular tachycardia, ventricular fibrillation and “torsade de pointes”.
When taken separately, both syndromes have little incidence, which leads us to expect this incidence to be even lower when they are found on the same electrocardiogram. Incidentally, the current medical literature contains no publications on this topic. This clinical case aims to establish the existence of an electrocardiographic pattern characterised by WPW and a PQTS pattern on an ECG record. With a high susceptibility to crisis of tachycardia, especially at night, several episodes of syncope, even cardiac arrest and sudden cardiac death.
The patient is a 24 old- years man. Since childhood, he has suffered from more than four tachycardia attacks, three documented syncope episodes, as well as two cardiac arrests recovered, for which he was treated with electric discharges. Afterwards, he was treated with radiofrequency ablation of Kent’s bundle, with permanent positive results so far.
We can see a typical ECG recording of an intermittent WPW and a Long QT-interval together in a patient with several syncopal episodes and a recovered cardiac arrest.
ECG patterns with short PR interval together to a long QT (A) and first-degree AV block alongside a long QT (B: Increased of cardiac electrical systole).
In this exposition, we present the ECG record of two patients with an obvious diversity and variability of alterations in the electrical system of heart. These electrical cardiac disturbances could explain completely the symptomatology from patients: nocturnal palpitations, several syncopal episodes. In Figure A, we can see the presence of a short PR-interval together to a Long QT-interval. In Figure B, we can also see an ECG recording with a Long PR-interval alongside a Long QT-interval.
Presence of a critical stenosis in left anterior descending coronary artery alongside a short “P-R” and “Q-T” pattern, in the same
electrocardiographic record.
The knowledge of the heart and its functions is increasing every day. However, many cardiac dysfunctions remain undocumented.
One of them might be the presence of the Wellens' sign, minimally elevated or isoelectric ST segments, and inverted T waves in the precordial leads, without changes in the QRS complex, together with a shortened of “P-R and Q-T intervals”
in the same electrocardiographic record. Both patterns are greatly underdiagnosed. The risk implied by the aforementioned underdiagnosis could have lethal consequences because the inherent problems in a short “P-R”-“Q-T” pattern could be added to those inherent in Wellens' sign.
Hereby, we set out to show both the description of the clinical case and the electrocardiogram (ECG) recording of a male having previously mentioned collection of symptoms.
The patient is a 42-year-old single man, previously diagnosed with unstable angina, who is an occasional smoker with arterial hypertension and who was prescribed
a felodipine (5 mg/d) and ramipril (5 mg/d) treatment.
The patient was complaining about an intense, oppressive, and progressive pain in the chest, which bore no relation to physical effort. The pain radiated toward both jaws and was accompanied by acute autonomic symptoms.
The sublingual administration of nitrates proved to be effective and led to a reduction of the pain as well as an improvement in the alterations the patient was showing. The ECG at presentation showed ST-segment elevations by more than 2 mm in all the precordial leads except lead one. The laboratory tests verified myocardial injury: L-lactate dehydrogenase, 1.220 UI/L (reference range, 230-460 UI/L);creatine kinase, 560 U/L (reference range, 37-290 U/L); creatine kinase], 1.85-14.45 U/L); aspartate transaminase, 376 U/L (reference range, 3-40 UI/L); alanine transaminase, 121 U/L (reference range, 5-37 UI/L); and troponin, 3.5 μg/L
(Reference range, 0-0.1 ng/mL).
In spite of the elevated biochemical markers of myocardial injury, the case was classified as an unstable angina variant.
The patient made full recovery as well as radical improvement of the clinical manifestations after the administration of nitrates (b30 minutes). As soon as the patient was clinically stabilized and the enzymatic levels regained their stability, the patient was discharged. He was also given a medical appointment in the hospital 10 days later so that he could be submitted to a new evaluation (We must add that, we do not know why the patient was not studied according to international guidelines during his first cardiac evaluation: angiography study within 24 hours at least). The patient showed no symptoms whatsoever when he returned home.
However, the patient returned to the hospital before his appointment was scheduled, describing similar symptoms to those, he had previously been afflicted by, but complaining, they were more acute and persistent.
That is the reason why the patient was automatically transferred to intensive care, where he was diagnosed with Wellens' sign.
After the patient was clinically and hemodynamically stabilized, he underwent a battery of diagnostic tests, which included an angiographic study, an echocardiogram and a single-photon emission computed tomography (SPECT) study.
Interestingly enough, the patient was reported to have had 3 short syncope attacks, from which he had fully recovered. He also had several nocturnal palpitation episodes, which were diagnosed as idiopathic supraventricular tachycardia.
As far as his family clinical history is concerned, an uncle on his father's side is known to have died of sudden death at the age of 46. His father had a history of acute coronary syndrome with ECG changes confined to the anterolateral leads.
The Wellens' sign represents an evolutionary stage of ST elevation acute coronary syndrome. Today, most of the patients are classified as non-ST elevation myocardial infarction, as they will have elevated troponin levels. Some patients are classified as unstable angina. The patients have similar symptoms: severe oppressive chest pain and radiation of the pain to different segments over a short period, but they usually respond to the administration of nitrates very quickly. Electrocardiographically speaking, the patients have very characteristic patterns: T-wave symmetrical inversion, with occasionally very deep T waves in precordial derivations, especially in V3 to V4, although these characteristics may extend to all the precordial derivations.
The Wellens' sign is associated with a critical stenosis in the left anterior descending coronary artery. Before the widespread implementation of invasive cardiology and effective antithrombotic therapy, 3 of 4 patients with this ECG pattern developed a usually extensive anterior myocardial infarction within a few weeks of admission. Our patient had bypass surgery.
Breijo et al. described the pattern of short “P-R and Q-T” intervals in 2008. It is characterized by the presence of an ECG with a P-R interval lesser than 0.12 seconds and the Q-T interval lesser than 0.350 seconds and, which, in more than 80% of cases, is accompanied by syncope episodes, nocturnal tachycardia, and occasionally, by ventricular fibrillation and even sudden death.
The key to an accurate diagnosis of both dysfunctions must begin with a detailed analysis of all the symptoms reported by the patient. The ECG recording provides an almost definitive confirmation:
The T-wave characteristics in precordial derivations.
The duration of P-R and Q-T intervals.
Typical image of ECG recording
THOUGHTS ABOUT THE PATTERNS DESCRIBED ABOVE:
All have a clear variation in the electrical cardiac systole.
All have a strong tendency to produce events of tachycardia / ventricular fibrillation.
Hence, all have a great capacity to produce cardiac arrest which, if not adequately diagnosed and treated, will inevitably occur sudden cardiac death.
REFERENCES
1. Brignole M, Alboni P, Benditt DG, Bergfeldt L, Blanc JJ, Bloch Thomsen PE, et al; Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope —update 2004. Europace. 2004;6:467-537.
2. Thijs RD, Benditt DG, Mathias CJ, Schondorf R, Sutton R, Wieling W, et al. Unconscious confusion —a literature search for definitions of syncope and related disorders. Clin Auton Res. 2005;15:35-9.
3. Soteriades ES, Evans JC, Larson MG, Chen MH, Chen L, Benjamin EJ, Levy D. Incidence and prognosis of syncope. N Engl J Med. 2002;347:878-85.
4. Strickberger SA, Benson DW, Biaggioni I, Callans DJ, Cohen MI, Ellenbogen KA, et al; American Heart Association Councils on Clinical Cardiology, Cardiovascular Nursing, Cardiovascular Disease in the Young, and Stroke; Quality of Care and Outcomes Research Interdisciplinary Working Group; American College of Cardiology Foundation; Heart Rhythm Society. AHA/ACCF scientific statement on the evaluation of syncope. J Am Coll Cardiol. 2006;47:473-84.
5. Hoefnagels WA, Padberg GW, Overweg J, Van der Velde EA, Roos RA. Transient loss of consciousness: the value of the history for distinguishing seizure from syncope. J Neurol. 1991;238:39-43.
6. Stephenson J. Fits and Faints. Oxford: Blackwell Scientific Publications; 1990. p. 41-57.
7. Van Dijk JG, Sheldon R. Is there any point to vasovagal syncope? Clin Auton Res. 2008;18:167-9.
8. Tea SH, Mansourati J, L’Heveder G, Mabin D, Blanc JJ. New insights into the pathophysiology of carotid sinus syndrome. Circulation. 1996;93:1411-6.
9. Alboni P, Alboni M, Bertorelle G. The origin of vasovagal syncope: to protect the heart or to escape predation? Clin Auton Res. 2008;18:170-8.
10. Mathias CJ, Mallipeddi R, Bleasdale-Barr K. Symptoms associated with orthostatic hypotension in pure autonomic failure and multiple system atrophy. J Neurol. 1999;246:893-8.
11. Naschitz J, Rosner I. Orthostatic hypotension: framework of the syndrome. Postgrad Med J. 2007;83:568-74.
12. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. J Neurol Sci. 1996;144:218-9.
13. Wieling W, Krediet P, Van Dijk N, Linzer M, Tschakovsky M. Initial orthostatic hypotension: review of a forgotten condition. Clin Sci (Lond). 2007;112:157-65.
14. Podoleanu C, Maggi R, Brignole M, Croci F, Incze A, Solano A, et al. Lower limb and abdominal compression bandages prevent progressive orthostatic hypotension in the elderly. A randomized placebo-controlled study. J Am Coll Cardiol. 2006;48:1425-32.
15. Gibbons CH, Freeman R. Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology. 2006;67:28-32.
16. Verheyden B, Gisolf J, Beckers F, Karemaker JM, Wesseling KH, Aubert A, et al. Impact of age on the vasovagal response provoked by sublingual nitroglycerine in routine tilt testing. Clin Sci (Lond). 2007;113:329-37.
17. Grubb BP, Kosinski DJ, Boehm K, Kip K. The postural orthostatic tachycardia syndrome: a neurocardiogenic variant identified during head-up tilt table testing. Pacing Clin Electrophysiol. 1997;20:2205-12.
18. Leitch JW, Klein GJ, Yee R, Leather RA, Kim YH. Syncope associated with supraventricular tachycardia: an expression of tachycardia or vasomotor response? Circulation. 1992;85:1064-71.
19. Brignole M, Gianfranchi L, Menozzi C, Raviele A, Oddone D, Lolli G, et al. Role of autonomic reflexes in syncope associated with paroxysmal atrial fibrillation. J Am Coll Cardiol. 1993;22:1123-9.
20. Ebert SN, Liu XK, Woosley RL. Female gender as a risk factor for drug-induced cardiac arrhythmias: evaluation of clinical and experimental evidence. J Womens Health. 1998;7:547-57.
21. Zareba W, Moss AJ, Le Cessie S, Locati EH, Robinson JL, Hall WJ, Andrews ML. Risk of cardiac events in family members of patients with Long QT syndrome. J Am Coll Cardiol. 1995;26:1685-91.
22. Lombroso CT, Lerman P. Breathholding spells (cyanotic and pallid infantile syncope). Pediatrics. 1967;39:563-81.
23. Wieling W, Ganzeboom KS, Saul JP. Reflex syncope in children and adolescents. Heart. 2004;90:1094-100.
24. Breijo-Marquez, F.R. Decrease of electrical cardiac systole. Int J. Cardiol. 2008;126:e36-8.
25. Breijo Marquez, FR. Pardo Ríos, M. Variability and diversity of electrical cardiac systole. BMJ Case Reports. 2009.
26. Breijo Marquez, FR. Pardo Ríos, M. Alcaraz Baños, M. Association of Short PR Interval, Long QT Interval, and Sudden Cardiac Death in a Young Male. Rev Esp Cardiol.2010; 63 :362-4.
27. Breijo-Márquez, FR. Pardo Rios, M. Presence of a critical stenosis in left anterior descending coronary artery alongside a short “P-R” and “Q-T” pattern, in the same electrocardiographic record. J Electrocardiology. 2010; 422-424.
28. Breijo-Marquez, FR. Pardo Ríos, M. Wolff-Parkinson-White and Prolonged “Q-T” Patterns in the Same Electrocardiographic Record. J Clinic Experiment Cardiol 2:118.
29. Breijo-Marquez, Fr. Pardo Ríos, M. Sudden cardiac death in a young adult with diagnosed with Tietze syndrome. Rev. Esp. Dolor. 2010. 56: 321-6
ACKNOWLEDGEMENTS
Lourdes and Alejandro Breijo, for their unselfishness collaboration from Miami. Florida. USA.
These inputs are intended only to sketch out some small notes about a subject so fascinating as is the heart study.
Wednesday, September 28, 2011
Thursday, August 25, 2011
Breijo II Pattern and Tako-Tsubo syndrome
The Tako-tsubo cardiomyopathy, also known as transient apical dysfunction, transient apical dyskinesia, stress-induced cardiomyopathy or broken heart syndrome, is a type of nonischemic cardiomyopathy in which there is a sudden temporary weakening of the myocardium.
The PR interval reflects the time the electrical impulse takes to travel from the sinus node through the AV node and entering the ventricles. The PR interval is therefore a good estimate of AV node function. Its normal values are between 0.120-0.200 seconds. When its length is lesser than 0.120 seconds, we speaking as a short PR-interval. This event has a great capacity for severe cardiac arrhythmia production.
Both entities can be very dangerous, separately. When they are together in the same individual, the consequences could be deadly.
The PR interval reflects the time the electrical impulse takes to travel from the sinus node through the AV node and entering the ventricles. The PR interval is therefore a good estimate of AV node function. Its normal values are between 0.120-0.200 seconds. When its length is lesser than 0.120 seconds, we speaking as a short PR-interval. This event has a great capacity for severe cardiac arrhythmia production.
Both entities can be very dangerous, separately. When they are together in the same individual, the consequences could be deadly.
Sunday, June 12, 2011
Wolff-Parkinson-White and Prolonged “Q-T” Patterns in the Same Electrocardiographic Record

Francisco R Breijo-Marquez1* and Pardo Ríos M2
1Department-in-Chief, Murcia University School of Medicine, Department of Clinical and Experimental Cardiology, University Campus.30100, Murcia, Spain
2Associate Professor of Cardiology, Murcia University School of Medicine, Department of Clinical and Experimental Cardiology, University Campus.30100, Murcia, Spain
*Corresponding author: Dr. Francisco R Breijo-Marquez
Murcia University School of Medicine
Department of Clinical and Experimental Cardiology
University Campus.30100, Murcia, Spain
Tel: 968681250 673517585
E-mail: frbreijo@aol.com
Received December 16, 2010; Accepted January 19, 2011; Published January 21, 2011
Citation: Breijo-Marquez FR, Pardo Ríos M (2011) Wolff-Parkinson-White and Prolonged “Q-T” Patterns in the Same Electrocardiographic Record. J Clinic Experiment Cardiol 2:118. doi:10.4172/2155-9880.1000118
Copyright: © 2011 Breijo-Marquez FR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Wolff-Parkinson-White syndrome (WPWS) is a congenital heart disease (PRKAG2. Genetic map 7q36) characterised by a premature ventricular depolarisation caused by an abnormal atrioventricular accessory pathway known as Kent’s bundle.
Prolonged QT syndrome (PQTS) consists of an abnormal prolongation of the QT interval on the ECG, which can be both inherited and acquired. This anomaly is known to favour the occurrence of malign cardiac arrhythmias, above all polymorphic ventricular tachycardia, ventricular fibrillation and “torsade de pointes”.
When taken separately, both syndromes have little incidence, which leads us to expect this incidence to be even lower when they are found on the same electrocardiogram. Incidentally, the current medical literature contains no publications on this topic. This clinical case aims to establish the existence of an electrocardiographic pattern characterised by WPW and a PQTS pattern on an ECG record. With a high susceptibility to crisis of tachycardia, especially at night, several episodes of syncope, even cardiac arrest.
The patient is a 24-year-old man. Since childhood, he has suffered from more than four tachycardia attacks, three documented syncope episodes, as well as two cardiac arrests recovered, for which he was treated with electric discharges. Afterwards, he was treated with radiofrequency ablation of Kent’s bundle, with permanent positive results so far (Figure 1).
Figure 1: Electro physiology Study. In the EPS graphic can be seen (arrow) typical signs of a WPW: Intracardiac electrogram showing under right ventricular pacing, atrial activation precocity in distal coronary sinus followed by His bundle.
Some Thoughts on this Case Report
Currently, our research team is working on features and management of this peculiar entity cardiology. Unfortunately, some are unknown to us yet.
The patient was positive for the gene of LQT1 (KCNQ1) (Figure 2).
He had not taken any medication to induce QT interval prolongation.
The fundamental symptoms were strong palpitations (especially at night), crises of severe tachycardia (greater than 250 bpm), episodes of syncope documented, with total reduction of consciousness, hypovolemic shock, reaching suffering two cardiac arrests.
The patient specific medication was never against the long QT, since he was never diagnosed with it: The long QT went unnoticed by your physicians. Our research team was who discovered to the two entities together in the same record ECG.
Although is a WPW intermittent, in all leads there is always a prolonged QT interval (values greater than 0.480 seconds), as can be measured in the ECG recording.
Following ablation, the patient has not suffered similar symptoms so far. Possibly this is because the patient is with sodium blockers as treatment, currently:
Your physicians chose the drug “hydroquinidine hydrochloride” against the WPW (a sodium blocker channels, class I) by orally. Because it has a stabilizing effect on the myocyte membrane and the capsule form with allows a stable absorption hydroquinidine for 8-12 hours and avoids the “peaks “in the hematic concentration of the substance. The maximum dose is 12.9mg/kg/ day, orally in two intakes each 12 hours. The dose is interrupted or reduced when the arrhythmia is eliminated or improved, or if hypotension occurs, the QRS complex widens by 50% or more, or the maximum dose is achieved.
The risks of intoxication or adverse effects are also lower.
Since the patient remains without symptoms following the radiofrequency ablation, we decided to maintain the current treatment but with strict control of the patient.
QT interval duration following the ablation was similar to the duration before ablation. Ie, a prolonged QT.
Figure 2: Electro cardiogram recording (12 leads). The presence of WPWS and PQTS can be observed.
Subscribe to:
Posts (Atom)